概要
The EasySep™ Human CD14 Positive Selection Kit II is designed to isolate highly purified CD14+ cells from fresh or previously frozen human peripheral blood mononuclear cells (PBMCs). Desired cells are targeted with Tetrameric Antibody Complexes recognizing CD14 and dextran-coated magnetic particles. Labeled cells are separated using an EasySep™ magnet without the use of columns. Cells of interest remain in the tube while unwanted cells are poured off. The CD14 antigen is strongly expressed on monocytes and macrophages and weakly on granulocytes. It is also expressed on most tissue macrophages.
This product replaces the EasySep™ Human CD14 Positive Selection Kit (Catalog #18058), for even faster cell isolations and is compatible with all EasySep™ magnets.
This product replaces the EasySep™ Human CD14 Positive Selection Kit (Catalog #18058), for even faster cell isolations and is compatible with all EasySep™ magnets.
技术资料
| Document Type | 产品名称 | Catalog # | Lot # | 语言 |
|---|---|---|---|---|
| Product Information Sheet | EasySep™ Human CD14 Positive Selection Kit II | 17858 | All | English |
| Product Information Sheet | RoboSep™ Human CD14 Positive Selection Kit II | 17858RF | All | English |
| Safety Data Sheet 1 | EasySep™ Human CD14 Positive Selection Kit II | 17858 | All | English |
| Safety Data Sheet 2 | EasySep™ Human CD14 Positive Selection Kit II | 17858 | All | English |
| Safety Data Sheet 1 | RoboSep™ Human CD14 Positive Selection Kit II | 17858RF | All | English |
| Safety Data Sheet 2 | RoboSep™ Human CD14 Positive Selection Kit II | 17858RF | All | English |
数据及文献
Data
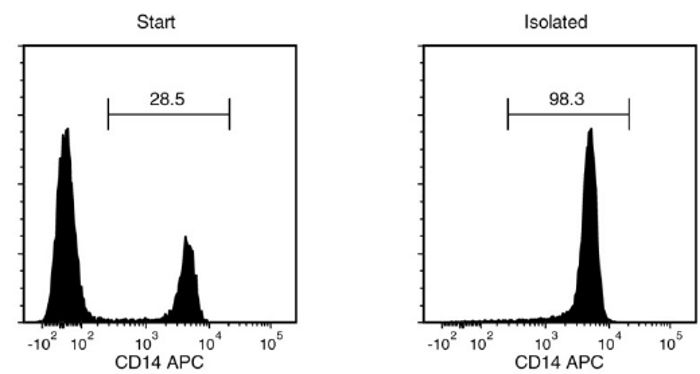
Figure 1. Typical EasySep™ Human CD14 Positive Selection II Isolation Profile
Starting with a single cell suspension of human PBMCs, the CD14+ cell content of the isolated fraction is typically 95.3 ± 4.5% (mean ± SD using the purple EasySep™ Magnet).
Publications (20)
Cell systems 2020 sep
Illuminating Host-Mycobacterial Interactions with Genome-wide CRISPR Knockout and CRISPRi Screens.
Abstract
Abstract
Existing antibiotics are inadequate to defeat tuberculosis (TB), a leading cause of death worldwide. We sought potential targets for host-directed therapies (HDTs) by investigating the host immune response to mycobacterial infection. We used high-throughput CRISPR knockout and CRISPR interference (CRISPRi) screens to identify perturbations that improve the survival of human phagocytic cells infected with Mycobacterium bovis BCG (Bacillus Calmette-Gu{\'{e}}rin), as a proxy for Mycobacterium tuberculosis (Mtb). Many of these perturbations constrained the growth of intracellular mycobacteria. We identified over 100 genes associated with diverse biological pathways as potential HDT targets. We validated key components of the type I interferon and aryl hydrocarbon receptor signaling pathways that respond to the small-molecule inhibitors cerdulatinib and CH223191, respectively; these inhibitors enhanced human macrophage survival and limited the intracellular growth of Mtb. Thus, high-throughput functional genomic screens, by elucidating highly complex host-pathogen interactions, can serve to identify HDTs to potentially improve TB treatment.
Cell 2020 nov
Detecting Tumor Antigen-Specific T Cells via Interaction-Dependent Fucosyl-Biotinylation.
Abstract
Abstract
Re-activation and clonal expansion of tumor-specific antigen (TSA)-reactive T cells are critical to the success of checkpoint blockade and adoptive transfer of tumor-infiltrating lymphocyte (TIL)-based therapies. There are no reliable markers to specifically identify the repertoire of TSA-reactive T cells due to their heterogeneous composition. We introduce FucoID as a general platform to detect endogenous antigen-specific T cells for studying their biology. Through this interaction-dependent labeling approach, intratumoral TSA-reactive CD4+, CD8+ T cells, and TSA-suppressive CD4+ T cells can be detected and separated from bystander T cells based on their cell-surface enzymatic fucosyl-biotinylation. Compared to bystander TILs, TSA-reactive TILs possess a distinct T cell receptor (TCR) repertoire and unique gene features. Although exhibiting a dysfunctional phenotype, TSA-reactive CD8+ TILs possess substantial capabilities of proliferation and tumor-specific killing. Featuring genetic manipulation-free procedures and a quick turnover cycle, FucoID should have the potential of accelerating the pace of personalized cancer treatment.
Science advances 2020 jun
Impact of mRNA chemistry and manufacturing process on innate immune activation.
Abstract
Abstract
Messenger RNA (mRNA) represents an attractive therapeutic modality for potentially a wide range of clinical indications but requires uridine chemistry modification and/or tuning of the production process to prevent activation of cellular innate immune sensors and a concomitant reduction in protein expression. To decipher the relative contributions of these factors on immune activation, here, we compared, in multiple cell and in vivo models, mRNA that encodes human erythropoietin incorporating either canonical uridine or N1-methyl-pseudouridine (1m$\Psi$), synthesized by either a standard process shown to have double-stranded RNA (dsRNA) impurities or a modified process that yields a highly purified mRNA preparation. Our data demonstrate that the lowest stimulation of immune endpoints was with 1m$\Psi$ made by the modified process, while mRNA containing canonical uridine was immunostimulatory regardless of process. These findings confirm that uridine modification and the reduction of dsRNA impurities are both necessary and sufficient at controlling the immune-activating profile of therapeutic mRNA.
Scientific reports 2020 feb
The anti-inflammatory potential of cefazolin as common gamma chain cytokine inhibitor.
Abstract
Abstract
A continuing quest for specific inhibitors of proinflammatory cytokines brings promise for effective therapies designed for inflammatory and autoimmune disorders. Cefazolin, a safe, first-generation cephalosporin antibiotic, has been recently shown to specifically interact with interleukin 15 (IL-15) receptor subunit $\alpha$ (IL-15R$\alpha$) and to inhibit IL-15-dependent TNF-$\alpha$ and IL-17 synthesis. The aim of this study was to elucidate cefazolin activity against IL-2, IL-4, IL-15 and IL-21, i.e. four cytokines sharing the common cytokine receptor $\gamma$ chain ($\gamma$c). In silico, molecular docking unveiled two potential cefazolin binding sites within the IL-2/IL-15R$\beta$ subunit and two within the $\gamma$c subunit. In vitro, cefazolin decreased proliferation of PBMC (peripheral blood mononuclear cells) following IL-2, IL-4 and IL-15 stimulation, reduced production of IFN-$\gamma$, IL-17 and TNF-$\alpha$ in IL-2- and IL-15-treated PBMC and in IL-15 stimulated natural killer (NK) cells, attenuated IL-4-dependent expression of CD11c in monocyte-derived dendritic cells and suppressed phosphorylation of JAK3 in response to IL-2 and IL-15 in PBMC, to IL-4 in TF-1 (erythroleukemic cell line) and to IL-21 in NK-92 (NK cell line). The results of the study suggest that cefazolin may exert inhibitory activity against all of the $\gamma$c receptor-dependent cytokines, i.e. IL-2, IL-4, IL-7, IL-9, IL-15 and IL-21.
Frontiers in immunology 2020
Fli1 Downregulation in Scleroderma Myeloid Cells Has Profibrotic and Proinflammatory Effects.
Abstract
Abstract
Scleroderma (SSc) is an autoimmune connective tissue disease characterized by immune dysregulation, vasculopathy, and fibrosis. We have previously demonstrated that low Fli1 expression in SSc fibroblasts and endothelial cells plays an important role in SSc pathogenesis. Cells of myeloid and lymphoid origin also express Fli1 and are dysregulated in patients with SSc, playing key roles in disease pathogenesis. However, the role for immune Fli1 in SSc is not yet clear. Our aim was to elucidate whether Fli1 contributes to the immune dysregulation seen in SSc. Comparison of the expression of Fli1 in monocytes, B- and T-cell fractions of PBMCs isolated from SSc patients and healthy controls (HC), showed an increase in Fli1 levels in monocytes. We used siRNA transfected human myeloid cells and mouse peritoneal macrophages obtained from Fli1 flox/flox LysMCre+/+ mice, and found that markers of alternative macrophage activation were increased with Fli1 deletion. Coculture of Fli1-deficient myeloid cells and primary human or mouse fibroblasts resulted in a potent induction of collagen type I, independent of TGF$\beta$ upregulation. We next analyzed global gene expression profile in response to Fli1 downregulation, to gain further insight into the molecular mechanisms of this process and to identify differentially expressed genes in myeloid cells. Of relevance to SSc, the top most upregulated pathways were hallmark IFN-$\gamma$ and IFN-$\alpha$ response. Additionally, several genes previously linked to SSc pathogenesis and fibrosis in general were also induced, including CCL2, CCL7, MMP12, and CXCL10. ANKRD1, a profibrotic transcription co-regulator was the top upregulated gene in our array. Our results show that Fli1-deficient myeloid cells share key features with cells from SSc patients, with higher expression of profibrotic markers and activation of interferon responsive genes, thus suggesting that dysregulation of Fli1 in myeloid cells may contribute to SSc pathogenesis.
The Journal of experimental medicine 2019 may
Thyrotropin aggravates atherosclerosis by promoting macrophage inflammation in plaques.
Abstract
Abstract
Subclinical hypothyroidism is associated with cardiovascular diseases, yet the underlying mechanism remains largely unknown. Herein, in a common population (n = 1,103), TSH level was found to be independently correlated with both carotid plaque prevalence and intima-media thickness. Consistently, TSH receptor ablation in ApoE-/- mice attenuated atherogenesis, accompanied by decreased vascular inflammation and macrophage burden in atherosclerotic plaques. These results were also observed in myeloid-specific Tshr-deficient ApoE-/- mice, which indicated macrophages to be a critical target of the proinflammatory and atherogenic effects of TSH. In vitro experiments further revealed that TSH activated MAPKs (ERK1/2, p38alpha, and JNK) and IkappaB/p65 pathways in macrophages and increased inflammatory cytokine production and their recruitment of monocytes. Thus, the present study has elucidated the new mechanisms by which TSH, as an independent risk factor of atherosclerosis, aggravates vascular inflammation and contributes to atherogenesis.

 网站首页
网站首页