概要
Learn more about our next-generation EasySep™ mouse cell isolation kits, featuring RapidSphere™ technology.
技术资料
| Document Type | 产品名称 | Catalog # | Lot # | 语言 |
|---|---|---|---|---|
| Product Information Sheet | EasySep™ Mouse Naïve CD4+ T Cell Isolation Kit | 19765 | All | English |
| Product Information Sheet | RoboSep™ Mouse Naïve CD4+ T Cell Isolation Kit | 19765RF | All | English |
| Safety Data Sheet 1 | EasySep™ Mouse Naïve CD4+ T Cell Isolation Kit | 19765 | All | English |
| Safety Data Sheet 2 | EasySep™ Mouse Naïve CD4+ T Cell Isolation Kit | 19765 | All | English |
| Safety Data Sheet 3 | EasySep™ Mouse Naïve CD4+ T Cell Isolation Kit | 19765 | All | English |
| Safety Data Sheet 1 | RoboSep™ Mouse Naïve CD4+ T Cell Isolation Kit | 19765RF | All | English |
| Safety Data Sheet 2 | RoboSep™ Mouse Naïve CD4+ T Cell Isolation Kit | 19765RF | All | English |
| Safety Data Sheet 3 | RoboSep™ Mouse Naïve CD4+ T Cell Isolation Kit | 19765RF | All | English |
数据及文献
Data
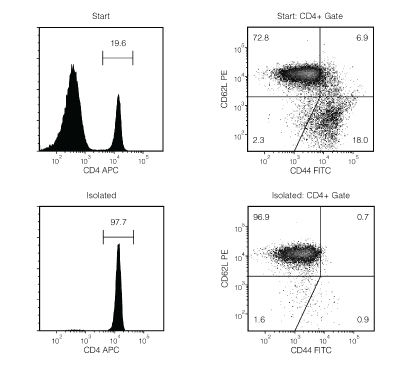
Figure 1. Typical EasySep™ Mouse Naïve CD4+ T Cell Isolation Profile
Starting with mouse splenocytes from an uninfected mouse, the naïve CD4+ T cell (CD4+CD44lowCD62Lhigh) content of the isolated fraction typically ranges from 89.9 - 95.6%. In the example above, the final purities of the start and isolated fractions are 14.3% and 94.7%, respectively.
 网站首页
网站首页




