概要
技术资料
| Document Type | 产品名称 | Catalog # | Lot # | 语言 |
|---|---|---|---|---|
| Product Information Sheet | MesenCult™ Adipogenic Differentiation Kit (Human) | 05412 | All | English |
| Safety Data Sheet 1 | MesenCult™ Adipogenic Differentiation Kit (Human) | 05412 | All | English |
| Safety Data Sheet 2 | MesenCult™ Adipogenic Differentiation Kit (Human) | 05412 | All | English |
| Safety Data Sheet 3 | MesenCult™ Adipogenic Differentiation Kit (Human) | 05412 | All | English |
数据及文献
Data
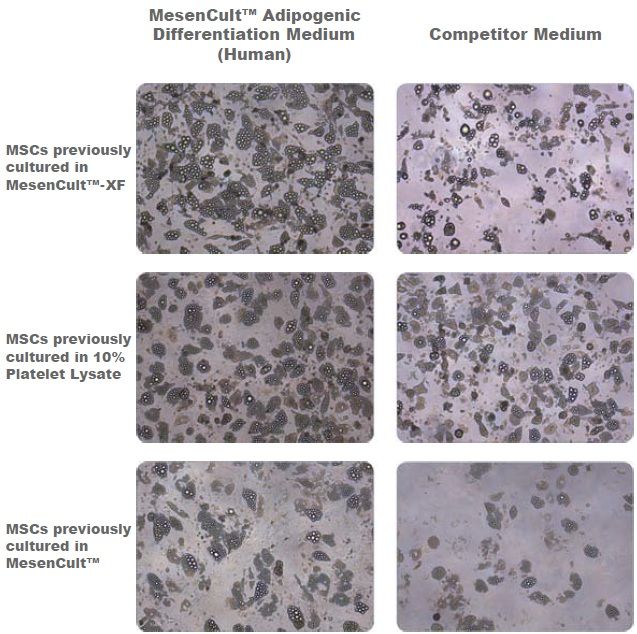
Figure 1. Adipogenic Differentiation of Human Bone Marrow-Derived MSCs
Adipogenic differentiation of human bone marrow-derived MSCs using MesenCult™ Adipogenic Differentiation Medium (Human) or a competitor medium. Prior to differentiation, MSCs were cultured for 2 passages in either serum- and xeno-free media (MesenCult™-XF or a 10% platelet lysate-based formulation) or serum-containing medium (MesenCult™) before undergoing differentiation. Even though differentation results are donor dependent, MesenCult™ Adipogenic Differentiation Medium (Human) consistently performed as well as, or better than the competitor medium. This trend was consistent for MSCs previously cultured in MesenCult™-XF, 10% Platelet Lysate or MesenCult™ medium.

 网站首页
网站首页