概要
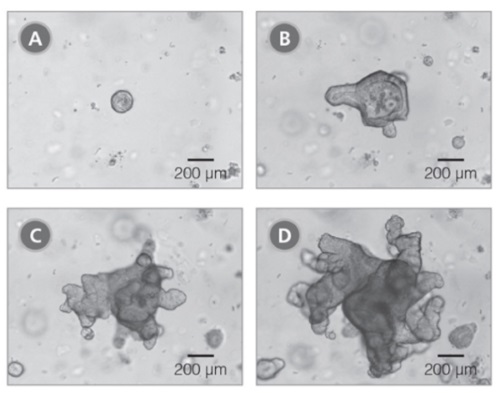
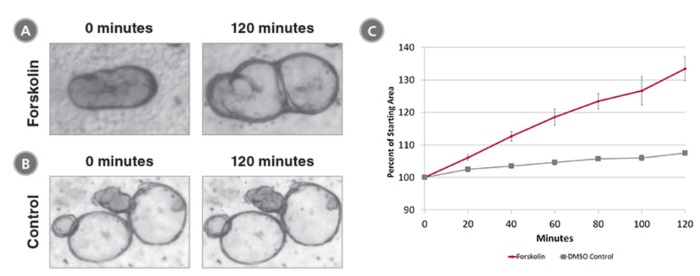
IntestiCult™ Organoid Growth Medium (Human) is a complete cell culture medium for efficient establishment and long-term maintenance of intestinal organoids derived from human intestinal crypts. Intestinal organoids provide a convenient in vitro organotypic culture system for studying the intestinal epithelium. The organoids incorporate a functional lumen enclosed by a polarized intestinal epithelial cell layer. Isolated intestinal crypts rapidly form organoids when cultured in IntestiCult™ Organoid Growth Medium (Human). Applications of intestinal organoid cultures include studying the development and function of intestinal epithelium, modeling intestinal diseases, and screening molecules for both efficacy and toxicity in an intestinal model. Intestinal organoid cultures can also be used for investigation of adult stem cell properties and for regenerative therapy approaches.
数据及文献
Publications (18)
ACS infectious diseases 2020 may
Fucose-Galactose Polymers Inhibit Cholera Toxin Binding to Fucosylated Structures and Galactose-Dependent Intoxication of Human Enteroids.
J. Cervin et al.
Abstract
A promising strategy to limit cholera severity involves blockers mimicking the canonical cholera toxin ligand (CT) ganglioside GM1. However, to date the efficacies of most of these blockers have been evaluated in noncellular systems that lack ligands other than GM1. Importantly, the CT B subunit (CTB) has a noncanonical site that binds fucosylated structures, which in contrast to GM1 are highly expressed in the human intestine. Here we evaluate the capacity of norbornene polymers displaying galactose and/or fucose to block CTB binding to immobilized protein-linked glycan structures and also to primary human and murine small intestine epithelial cells (SI ECs). We show that the binding of CTB to human SI ECs is largely dependent on the noncanonical binding site, and interference with the canonical site has a limited effect while the opposite is observed with murine SI ECs. The galactose-fucose polymer blocks binding to fucosylated glycans but not to GM1. However, the preincubation of CT with the galactose-fucose polymer only partially blocks toxic effects on cultured human enteroid cells, while preincubation with GM1 completely blocks CT-mediated secretion. Our results support a model whereby the binding of fucose to the noncanonical site places CT in close proximity to scarcely expressed galactose receptors such as GM1 to enable binding via the canonical site leading to CT internalization and intoxication. Our finding also highlights the importance of complementing CTB binding studies with functional intoxication studies when assessing the efficacy inhibitors of CT.
Nature communications 2020 may
TNFAIP8 controls murine intestinal stem cell homeostasis and regeneration by regulating microbiome-induced Akt signaling.
J. R. Goldsmith et al.
Abstract
The intestine is a highly dynamic environment that requires tight control of the various inputs to maintain homeostasis and allow for proper responses to injury. It was recently found that the stem cell niche and epithelium is regenerated after injury by de-differentiated adult cells, through a process that gives rise to Sca1+ fetal-like cells and is driven by a transient population of Clu+ revival stem cells (revSCs). However, the molecular mechanisms that regulate this dynamic process have not been fully defined. Here we show that TNFAIP8 (also known as TIPE0) is a regulator of intestinal homeostasis that is vital for proper regeneration. TIPE0 functions through inhibiting basal Akt activation by the commensal microbiota via modulating membrane phospholipid abundance. Loss of TIPE0 in mice results in injury-resistant enterocytes, that are hyperproliferative, yet have regenerative deficits and are shifted towards a de-differentiated state. Tipe0-/- enterocytes show basal induction of the Clu+ regenerative program and a fetal gene expression signature marked by Sca1, but upon injury are unable to generate Sca-1+/Clu+ revSCs and could not regenerate the epithelium. This work demonstrates the role of TIPE0 in regulating the dynamic signaling that determines the injury response and enables intestinal epithelial cell regenerative plasticity.
Toxicology in vitro : an international journal published in association with BIBRA 2020 jul
Human ileal organoid model recapitulates clinical incidence of diarrhea associated with small molecule drugs.
D. G. Belair et al.
Abstract
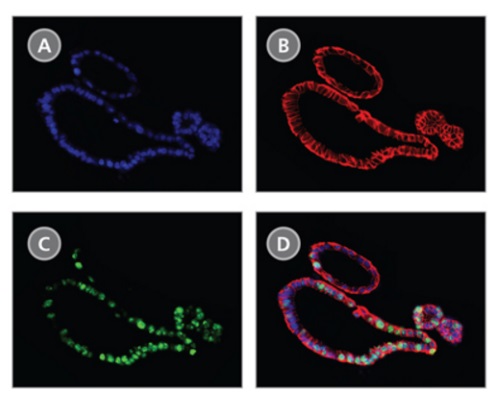
Drug-induced gastrointestinal toxicity (GIT) is a common treatment-emergent adverse event that can negatively impact dosing, thereby limiting efficacy and treatment options for patients. An in vitro assay of GIT is needed to address patient variability, mimic the microphysiology of the gut, and accurately predict drug-induced GIT. Primary human ileal organoids (termed 'enteroids') have proven useful for stimulating intestinal stem cell proliferation and differentiation to multiple cell types present in the gut epithelium. Enteroids have enabled characterization of gut biology and the signaling involved in the pathogenesis of disease. Here, enteroids were differentiated from four healthy human donors and assessed for culture duration-dependent differentiation status by immunostaining for gut epithelial markers lysozyme, chromogranin A, mucin, and sucrase isomaltase. Differentiated enteroids were evaluated with a reference set of 31 drugs exhibiting varying degrees of clinical incidence of diarrhea, a common manifestation of GIT that can be caused by drug-induced thinning of the gut epithelium. An assay examining enteroid viability in response to drug treatment demonstrated 90{\%} accuracy for recapitulating the incidence of drug-induced diarrhea. The human enteroid viability assay developed here presents a promising in vitro model for evaluating drug-induced diarrhea.
The Journal of clinical investigation 2020 jan
Apelin directs endothelial cell differentiation and vascular repair following immune-mediated injury.
A. G. Masoud et al.
Abstract
Sustained, indolent immune injury of the vasculature of a heart transplant limits long-term graft and recipient survival. This injury is mitigated by a poorly characterized, maladaptive repair response. Vascular endothelial cells respond to proangiogenic cues in the embryo by differentiation to specialized phenotypes, associated with expression of apelin. In the adult, the role of developmental proangiogenic cues in repair of the established vasculature is largely unknown. We found that human and minor histocompatibility-mismatched donor mouse heart allografts with alloimmune-mediated vasculopathy upregulated expression of apelin in arteries and myocardial microvessels. In vivo, loss of donor heart expression of apelin facilitated graft immune cell infiltration, blunted vascular repair, and worsened occlusive vasculopathy in mice. In vitro, an apelin receptor agonist analog elicited endothelial nitric oxide synthase activation to promote endothelial monolayer wound repair and reduce immune cell adhesion. Thus, apelin acted as an autocrine growth cue to sustain vascular repair and mitigate the effects of immune injury. Treatment with an apelin receptor agonist after vasculopathy was established markedly reduced progression of arterial occlusion in mice. Together, these initial data identify proangiogenic apelin as a key mediator of coronary vascular repair and a pharmacotherapeutic target for immune-mediated injury of the coronary vasculature.
Journal of animal science 2020 feb
Evaluation of swine enteroids as in vitro models for Lawsonia intracellularis infection1,2.
T. P. Resende et al.
Abstract
The enteric pathogen Lawsonia intracellularis is one of the main causes of diarrhea and compromised weight gain in pigs worldwide. Traditional cell-line cultures have been used to study L. intracellularis pathogenesis. However, these systems fail to reproduce the epithelial changes observed in the intestines of L. intracellularis-infected pigs, specifically, the changes in intestinal cell constitution and gene expression. A more physiologically accurate and state-of-the-art model is provided by swine enteroids derived from stem cell-containing crypts from healthy pigs. The objective of this study was to verify the feasibility of two-dimensional swine enteroids as in vitro models for L. intracellularis infection. We established both three- and two-dimensional swine enteroid cultures derived from intestinal crypts. The two-dimensional swine enteroids were infected by L. intracellularis in four independent experiments. Enteroid-infected samples were collected 3 and 7 d postinfection for analysis using real-time quantitative PCR and L. intracellularis immunohistochemistry. In this study, we show that L. intracellularis is capable of infecting and replicating intracellularly in two-dimensional swine enteroids derived from ileum.
mBio 2020
Genetic Manipulation of Human Intestinal Enteroids Demonstrates the Necessity of a Functional Fucosyltransferase 2 Gene for Secretor-Dependent Human Norovirus Infection.
K. Haga et al.
Abstract
Human noroviruses (HuNoVs) are the leading cause of nonbacterial gastroenteritis worldwide. Histo-blood group antigen (HBGA) expression is an important susceptibility factor for HuNoV infection based on controlled human infection models and epidemiologic studies that show an association of secretor status with infection caused by several genotypes. The fucosyltransferase 2 gene (FUT2) affects HBGA expression in intestinal epithelial cells; secretors express a functional FUT2 enzyme, while nonsecretors lack this enzyme and are highly resistant to infection and gastroenteritis caused by many HuNoV strains. These epidemiologic associations are confirmed by infections in stem cell-derived human intestinal enteroid (HIE) cultures. GII.4 HuNoV does not replicate in HIE cultures derived from nonsecretor individuals, while HIEs from secretors are permissive to infection. However, whether FUT2 expression alone is critical for infection remains unproven, since routinely used secretor-positive transformed cell lines are resistant to HuNoV replication. To evaluate the role of FUT2 in HuNoV replication, we used CRISPR or overexpression to genetically manipulate FUT2 gene function to produce isogenic HIE lines with or without FUT2 expression. We show that FUT2 expression alone affects both HuNoV binding to the HIE cell surface and susceptibility to HuNoV infection. These findings indicate that initial binding to a molecule(s) glycosylated by FUT2 is critical for HuNoV infection and that the HuNoV receptor is present in nonsecretor HIEs. In addition to HuNoV studies, these isogenic HIE lines will be useful tools to study other enteric microbes where infection and/or disease outcome is associated with secretor status.IMPORTANCE Several studies have demonstrated that secretor status is associated with susceptibility to human norovirus (HuNoV) infection; however, previous reports found that FUT2 expression is not sufficient to allow infection with HuNoV in a variety of continuous laboratory cell lines. Which cellular factor(s) regulates susceptibility to HuNoV infection remains unknown. We used genetic manipulation of HIE cultures to show that secretor status determined by FUT2 gene expression is necessary and sufficient to support HuNoV replication based on analyses of isogenic lines that lack or express FUT2. Fucosylation of HBGAs is critical for initial binding and for modification of another putative receptor(s) in HIEs needed for virus uptake or uncoating and necessary for successful infection by GI.1 and several GII HuNoV strains.
View All Publications
 网站首页
网站首页